sponsor content What's this?

From data to delivery: A path to value-based health care for VA and DoD
Looking to commercial best practices to help the Departments of Defense and Veterans Affairs transition to value-based care.
Presented by
Optum

With health care expenditures approaching nearly 25 percent of Gross Domestic Product (GDP), government agencies and organizations throughout the country are in need of innovative solutions that stem the tide of rising health care costs, while also improving the quality of care and patient experiences.
This is especially true for millions of our nation’s heroes who receive some or all of their care through the Military Health System (MHS) and the Veterans Health Administration (VHA). Because of the sheer size of these systems, in terms of geographic reach and lives covered, and in consideration that each organization must manage costs and quality as both a payer and a provider, efforts to provide unfettered access to high-value, highly reliable care often reflect some of the most daunting challenges seen across the American health system.
To address these challenges, both the Defense Health Agency (DHA) and the VHA have emphasized integration of system capabilities to create highly dependable health systems in a series of coordinated, data-driven initiatives that focus on value by prioritizing quality and safety, eliminating waste and reducing unwarranted variation to better serve Military Service Members, Veterans and their beneficiaries.
Recent legislation, such as the National Defense Authorization Act of 2017 and the VA MISSION Act of 2018, has taken steps to address these challenges by introducing value-based payments models within agencies like the Departments of Defense (DOD) and Veterans Affairs (VA) through authorizing a series of pilot programs.
Understanding the basics: What exactly are value-based payments?
The most important thing to know about value-based care is that it puts the patient at the center of the health care experience ensuring quality at every step of the process. To fully transition to this type of model it will require additional attention to every aspect of the service to ensure that quality is continuously improved, which reduces costs for patients and providers.
For decades, the health care system has evolved in a way that pays health care providers for the volume of patients they treat, not necessarily the value they provide. Despite spending two times what most other developed nations spend on a per capita basis for health care, the United States has a greater prevalence of chronic disease and overall poorer health outcomes, as well as higher costs for health care services.
Changing the payment model from the current fee-for-service (FFS) model, which reimburses services regardless of outcome, to a value-based payment model, which reimburses outcomes regardless of the services delivered, is a step in the right direction.
The Centers for Medicaid and Medicare Services (CMS) defines value-based payments for Medicare as “programs that reward health care providers with incentives for the quality of care they give to patients.” Value-based care programs are targeted to support the three tenets to deliver:
- Better care for individuals
- Better health for populations
- Lower cost CMS
further defines value-based payments through its Medicaid Innovation Accelerator Program as “payment models that range from rewarding for performance in fee-for-service (FFS) to capitation” and “ties provider payment directly to specific indicators of quality or efficiency and can be built through rewards and penalties.”
Leveraging experience from commercial value-based care programs
Commercial payers faced with the challenge to deliver improved care at lower costs have found ways to incorporate value-based care concepts into the current reimbursement systems and then, after gaining experience, have transitioned to models where FFS is no longer the basis of payment.
Figure 1 provides an overview of several different value-based care models, each model’s high-level objective and notes to consider when implementing.
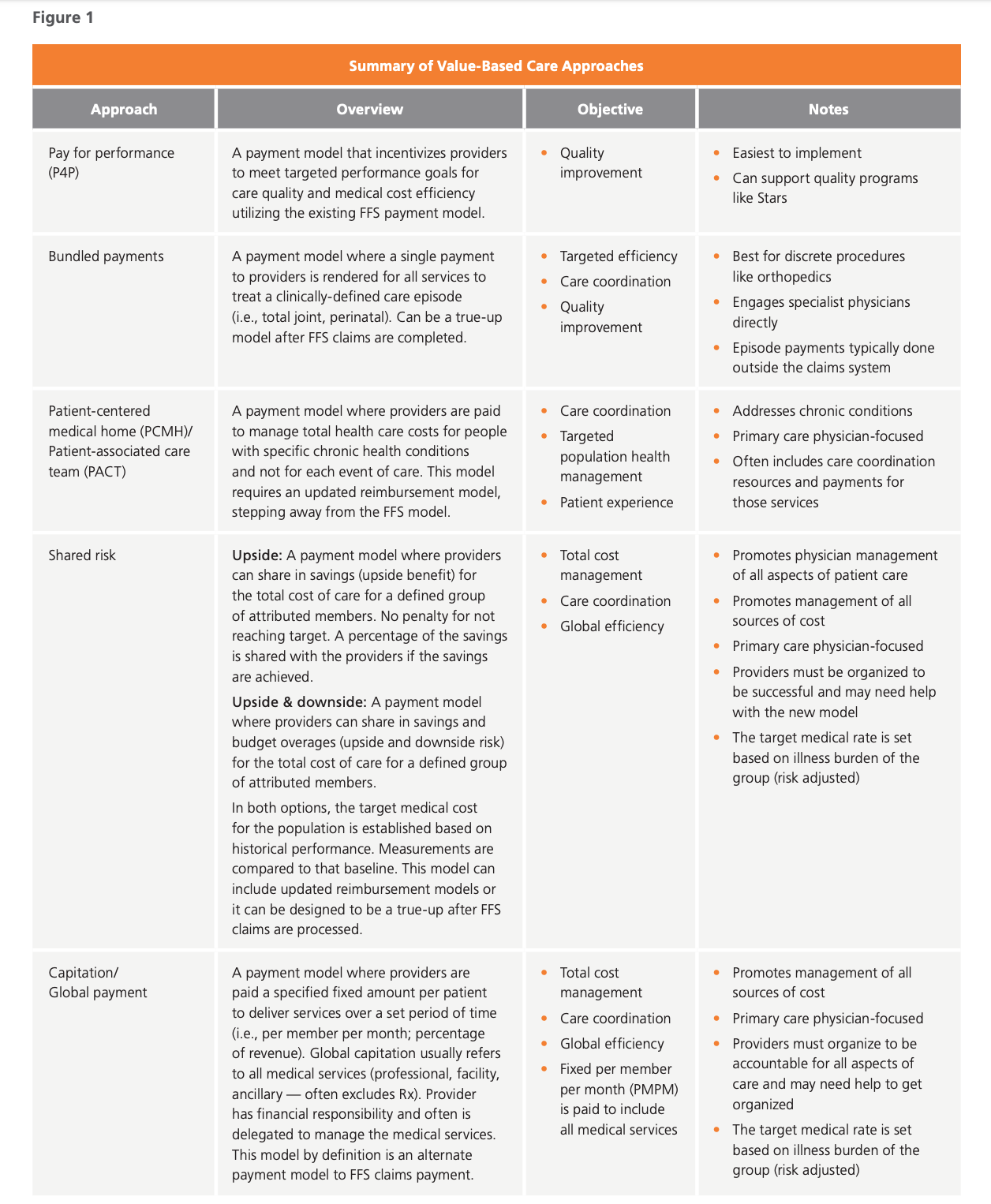
Results from the commercial market have shown that many delivery systems have not yet built the fundamental processes and capabilities necessary to successfully take on risk and/or move to mature value-based payment models such as capitation. Many organizations, such as UnitedHealth Group®, see significant value in value-based care and are creating a path to better health, better care and lower costs — for everyone.
UnitedHealth Group, which includes both Optum® and UnitedHealthcare® (the largest health insurance company in America) has more than 15 million members receiving care from health professionals who participate in value-based arrangements. Operating over 1,000 accountable care organizations within a network of care providers, over 110,000 physicians and 1,100 hospitals participate in UnitedHealthcare’s value-based care programs. These programs are intended to help people lead healthier lives by giving them and their doctors evidence-based health guidelines that result in improved outcomes at lower costs and incentives that reward more coordinated care.
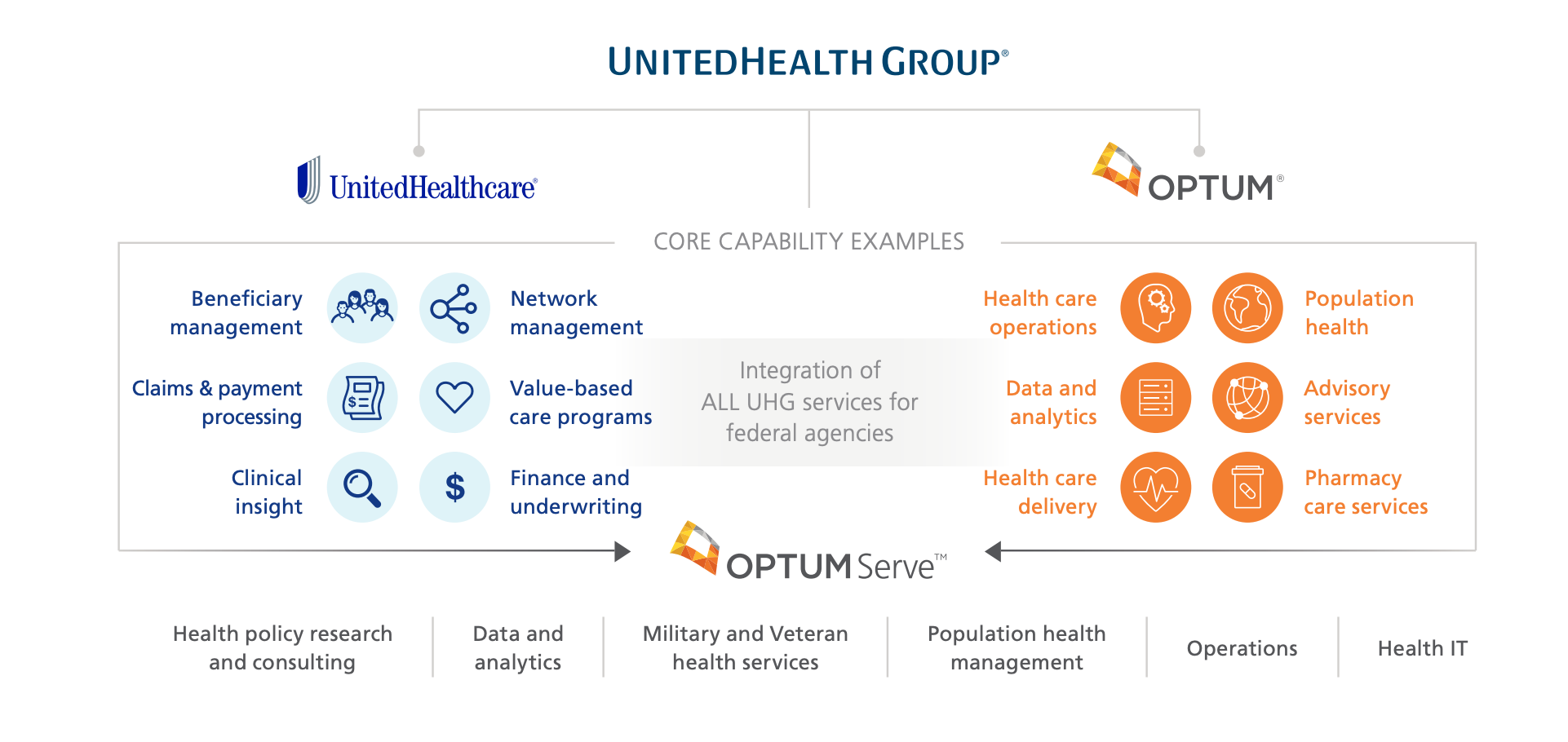
UnitedHealthcare currently delivers $73 billion in annual payments through contracts containing valuebased features, with the goal of $75 billion by the end of 2020. As a result, UnitedHealthcare and care providers in value-based relationships have worked together to identify and close 50 million gaps in care from 2013 through 2018. Lessons learned from the commercial space by UnitedHealthcare, combined with the federal experience of OptumServeTM (the federal health business of Optum and UnitedHealth Group) could help identify ways to ease the transition to value-based care for the Departments of Defense and Veterans Affairs.
Considerations for VHA and DHA
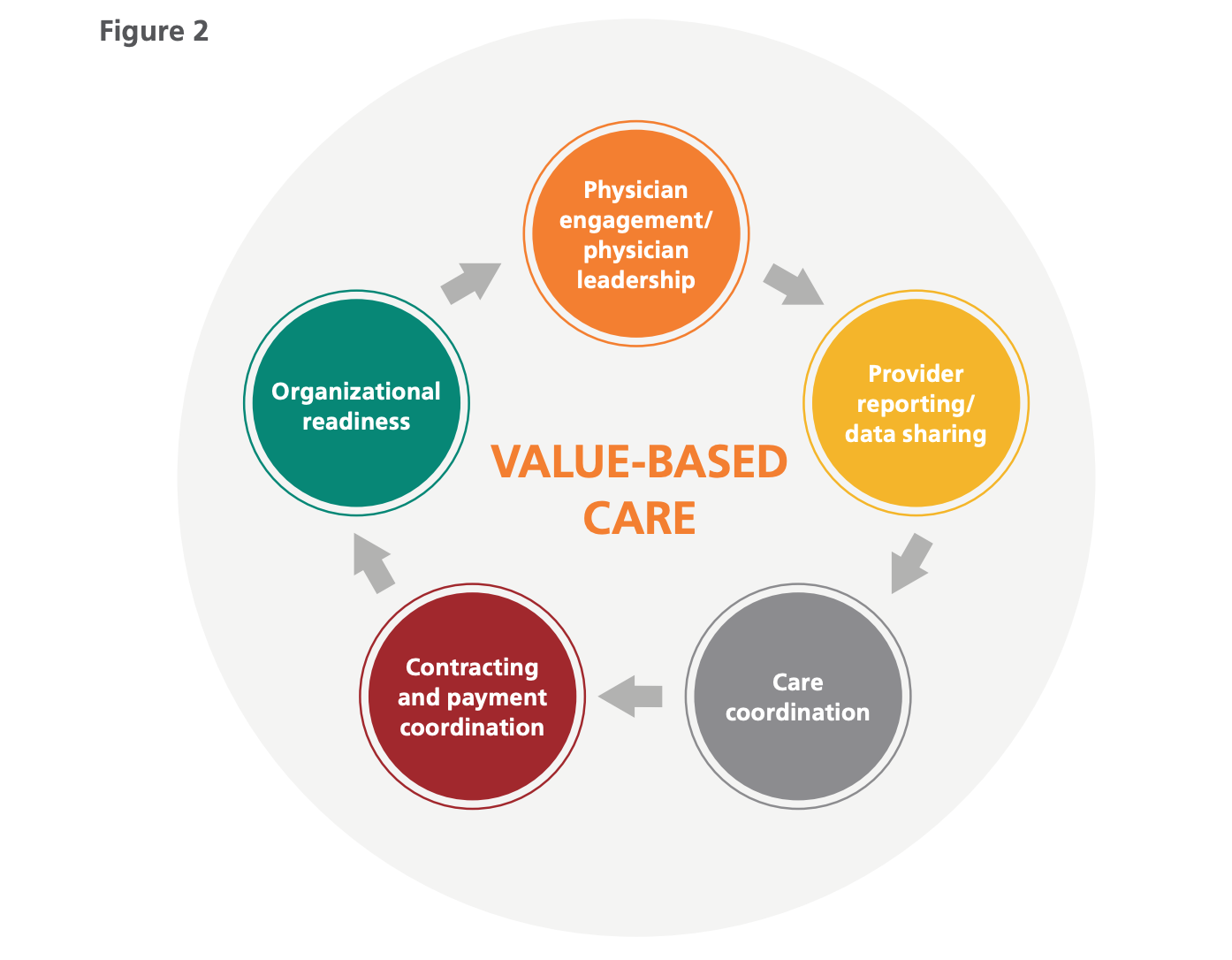
Optum and UnitedHealthcare have participated in several value-based payment programs that have had an overall favorable impact on total costs and patient quality both in the United States and internationally. Through the participation and management of these programs, there are several lessons learned that decision-makers at DOD and VA could consider in planning similar efforts. A successful value-based payment program has several integrated components, as seen in Figure 2, with various tasks and activities within each. Each component contributes to the success of the value-based payment program.
For example:
- Physician engagement/physician leadership: Physician leadership is a critical success factor as this type of change requires commitment and investment by physicians to be successful. It is important to structure attractive programs and payment methods to ensure physicians continue to learn and contribute to improving the delivery of care.
- Provider reporting/data sharing: Data sharing and provider reporting are important features of successful programs because improvements to care are structured from fact-based evidence. It is crucial to develop informative provider reporting for all aspects of care improvement. There can be challenges sharing information across networks (from primary care to specialty care). Preparing to handle the movement and sharing of data is necessary, including security to ensure patient safety.
- Care coordination: Value-based care models require efficient patient movement from one aspect of care to the next. Many successful organizations have added care coordination resources to guide that movement to ensure that care and financial targets can be met and that care is never delayed for any reason.
- Contracting and payment coordination: As with all changes to reimbursement, provider contracts will require amendments addressing the components of any new model. Payment systems for both providers and payers may need to be augmented to handle the additional payments presented with value-based care models.
- Organizational readiness: Several of the risk-based models require a sufficient beneficiary population to be credibly measured and produce stable results year over year. During the organizational readiness assessment, factors such as membership should be taken into consideration to determine the possible resources needed and outcomes to be achieved.
Analytics, incremental changes and program strategy are essential
With all risk-sharing arrangements, especially value-based payment models, analytics are pivotal to building the care and cost benchmarks. The federal health systems will want to maintain strong oversight and accountability and make data-driven decisions as they innovate and optimize. Addressing these two needs, Optum maintains a secure and reliable database covering nearly 240 million de-identified lives of data (spanning clinical, claims and employer benefits) used to foster innovation and research across health care. In combination with the approximately $3.6 billion of annual investment that UnitedHealth Group provides in technology and innovation, Optum can provide insights on how to best migrate to value-based care and optimize the model to provide the highest quality of care. For example, if a practice that has migrated to a value-based care model discovers areas that are not improving, by leveraging Optum analytics they can have access to actionable intelligence that drives the understanding on why the practice has failed to hit key benchmarks. Optum, through its use of data and analytics tools, can predict cases that are meeting or exceeding expectations and cases that show risk for immediate intervention. Optum analytics can also recommend the most effective providers through data analysis of provider delivery history.
Value-based care requires analysis that identifies specific clinical actions that apply meaningful insights to positively influence quality measures. Bringing together data from multiple sources requires precise curation to support the analytics needed for a value-based care program to be successful. Optum has the ability to curate large amounts of data from multiple, disparate sources to bring forward operational and predictive analyses to improve care delivery and also improve the effectiveness of the value-based care program, as seen in Figure 3.
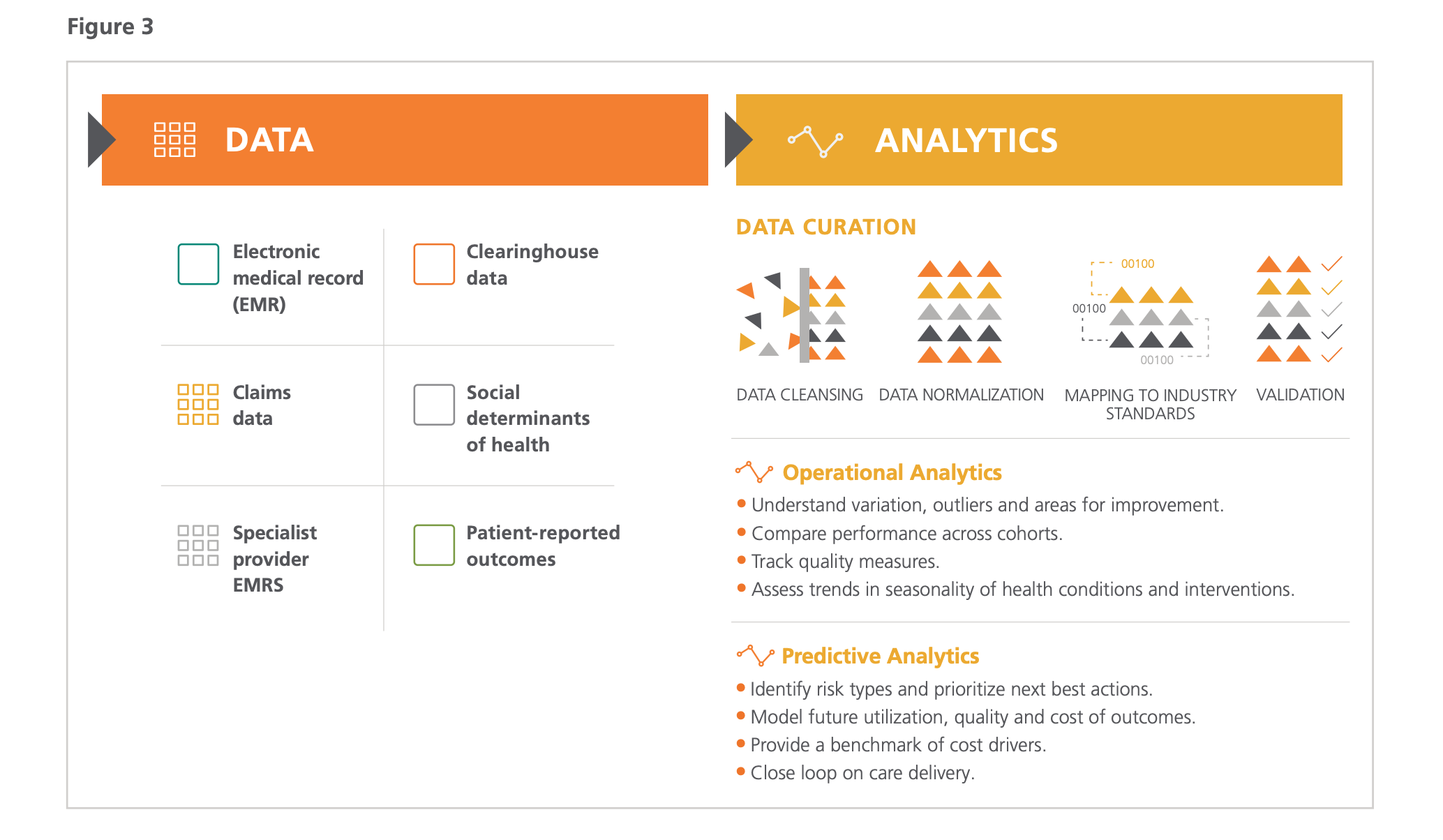
As the VHA and DHA look to move to more value-based payment models, one of the critical areas of transition is the sharing of data to improve outcomes. To mitigate the impact of transitioning to value-based care, the VHA and DHA can select models that work with the current fee-for-service and data management platforms and migrate to more complex and mature paradigms over time as those capabilities mature. Without completely reengineering the payment systems, incremental changes can drive a focus on the measurement of outcomes and help each agency’s leadership plan the transition to value-based payments without compromising the care or experience they provide.
Many, if not most, organizations looking to implement value-based care models run into challenges. These are often the routine challenges to scale that can be avoided or worked through with the support of experienced change management consultants and operational designers. OptumServe has experience working across the federal health ecosystem to clearly define program strategy in a way that aligns with both the payer (DOD or VA) and the provider. OptumServe is able to support federal agencies by bringing commerical experience to government health care to align care pathways, support operational and financial administration processes, and develop and deliver accurate reporting on value-based programs.
Experience matters: Choose the right partner
One critical step toward actualizing value-based care is partnering with an organization that not only has the experience in both the public and the private sectors to drive the best solutions for an agency, but the data, experience and access to physicians that help agencies navigate the steps needed to transition to a value-based care model.
Indeed, implementation requires experience and scalability. Optum is the largest employer of physicians and nurses in the United States, and it manages provider practices so while they consult with commercial payers, they are also implementing value-based care across their clinical landscape — no other commercial company has this capability.
Agencies can ease the transition to value-based care with Optum helping to develop an end-to-end strategy that includes creating an achievable plan to bend the cost curve, satisfy patients and deliver better health outcomes. It is one of the best ways that Veterans, Military Service Members and others can get improved levels of care while also minimizing the cost burden on agencies responsible for those treatments. Those lower costs can then be reinvested back into the care delivery system, allowing federal health care providers to treat more patients more efficiently, and provide an optimal level of care with a positive patient experience. Optum stands ready to help the Defense Health Agency and the Department of Veterans Affairs develop and deliver better health outcomes for our heroes.
About Optum
Optum is a leading health services innovation company dedicated to helping make the health system work better for everyone. With more than 190,000 people worldwide, Optum combines technology, data and expertise to improve the delivery, quality and efficiency of health care. Optum uniquely collaborates with all participants in health care, connecting them with a shared focus on creating a healthier world. Hospitals, doctors, pharmacies, employers, health plans, government agencies and life sciences companies rely on Optum services and solutions to solve their most complex challenges and meet the growing needs of the people and communities they serve.
About OptumServe
OptumServe is the federal health services business of Optum and UnitedHealth Group (NYSE: UNH). We are proud to partner with the Departments of Defense, Health and Human Services, Veterans Affairs and other organizations to help modernize the U.S. health system and improve the health and well-being of those we collectively serve.
NEXT STORY: Transforming Facilities Management with a Business-Inspired Approach