3D bioprinting: Repairing burns, other traumatic injuries with new cells
Army researchers, part of a consortium of universities, hospitals and others, work on printing healthy cells onto serious wounds.
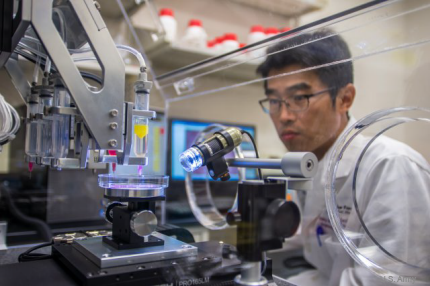
A researcher works on a project for bioprinting muscle tissue.
Safety improvements for soldiers on the battlefield—better body armor and vehicle design, along with advanced field medical treatments—mean soldiers are surviving injuries that would have killed them decades ago. But those injuries, such as serious burns and tissue damage caused by roadside bombs, are traumatic, debilitating and often permanent.
That led the Defense Department to invest in research into regenerative medicine, to find new ways of restoring damaged cells, tissues and organs. In 2008, DOD established the Armed Forces Institute of Regenerative Medicine, or AFIRM, a consortium of about 30 universities, hospitals and other partners, led by the Wake Forest Institute for Regenerative Medicine.
One technology showing promise is 3D printing, specifically 3D bioprinting, which is capable of precisely applying healthy cells to a wounded area, according to an Army report. The cells can then grow to create new skin.
"There was an increasing need to deliver therapies for wounded warriors” Dr. Michael Romanko of the Tissue Injury and Regenerative Medicine Project Management Office within the U.S. Army Medical Material Development Activity, said in the report. “We saw a spike in the severity of the trauma that these soldiers were receiving. As we increased the quality of battle armor, the injuries they were surviving were that much more debilitating."
Burns account for 10 percent to 30 percent of battlefield casualties, the Army said, and in recent years improvised explosive devices have caused serious injuries to an increasing number of soldiers. 3D bioprinting would allow doctors to tailor their treatment to each patient.
In a scenario Romanko gave, scientist would take a laser scan of a badly burned area and create a 3D map of the area. A computer program interprets the map and tells the scientists what types of cells to use. They then load the bioprinter (which works like a laser jet printer) with two types of cells—fibroblasts for the deeper layer of skin and keratinocytes for the surface layer. The printer places the cells precisely, and the cells grow into skin, complete with sweat glands, hair follicles and proper pigmentation.
The researchers aren’t all the way there yet, but said their early effort show promise. Beyond recreating skin, research also is being conducted into vascular bioprining that could lead to creating organs, muscle tissue and even limbs. Scientist at the Wake Forest institute have experimented with printing the structures of body parts, including a finger, ear and kidney.

The structure for a kidney, ear and finger bone printed at Wake Forest.
Working with the consortium lets the Army collaborate with a number of specialists to advance the various aspects of the research, including the imaging technology, the printers and tissue and organ repair. Eventually, the researchers hope bioprinting can become a viable, common treatment.
"This has very widespread use, not only to the military audience, but also to the civilian population,” Romanko said. “We need a larger commercialization audience in order to be a self-sustaining technology."
In addition to the Army, AFIRM gets funding from the Office of Naval Research, Air Force Surgeon General's Office, Veterans Health Administration, National Institutes of Health and the Office of Assistant Secretary of Defense for Health Affairs, as well as from other federal, state and private sources.