
HANNA BARCZYK AND FRANZISKA BARCZYK
How the Coronavirus Became an American Catastrophe
The death and economic damage sweeping the United States could have been avoided—if only we had started testing for the virus sooner.
How many people are sick with the coronavirus in the United States, and when did they get sick?
These are crucial questions to answer, but they have never been answered well. Archived data from the Centers for Disease Control and Prevention—illustrated in the chart below—reveal that the government dramatically misunderstood what was happening in America as the outbreak began.
On the last day of February, the CDC reported that 15 Americans had tested positive for COVID-19, the disease caused by the coronavirus.
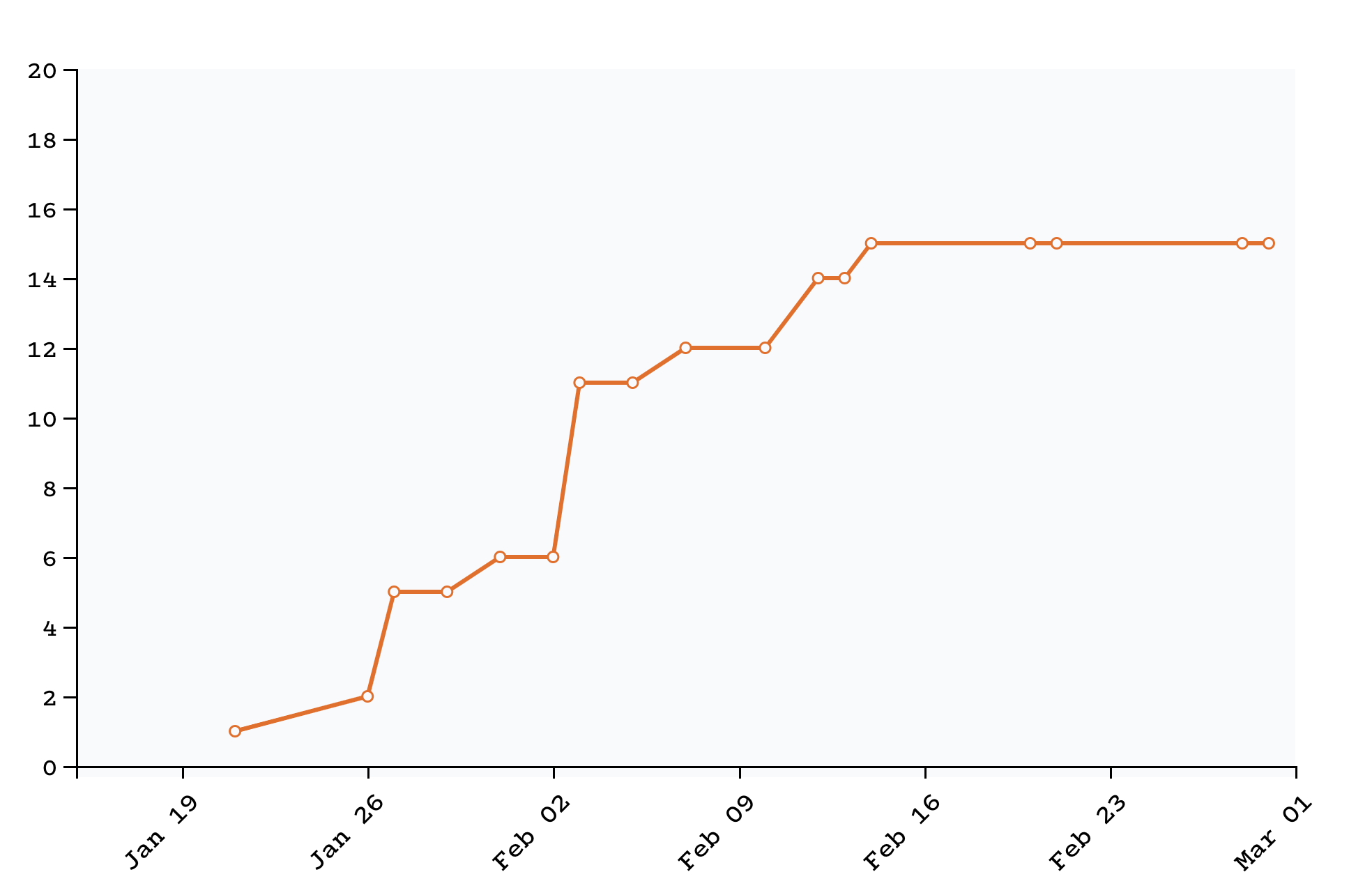
Data: The Internet Archive’s cache of CDC.gov
In the past week, as the country’s testing capacity has increased, officials have discovered more cases. Today, more than 17,000 people have tested positive.
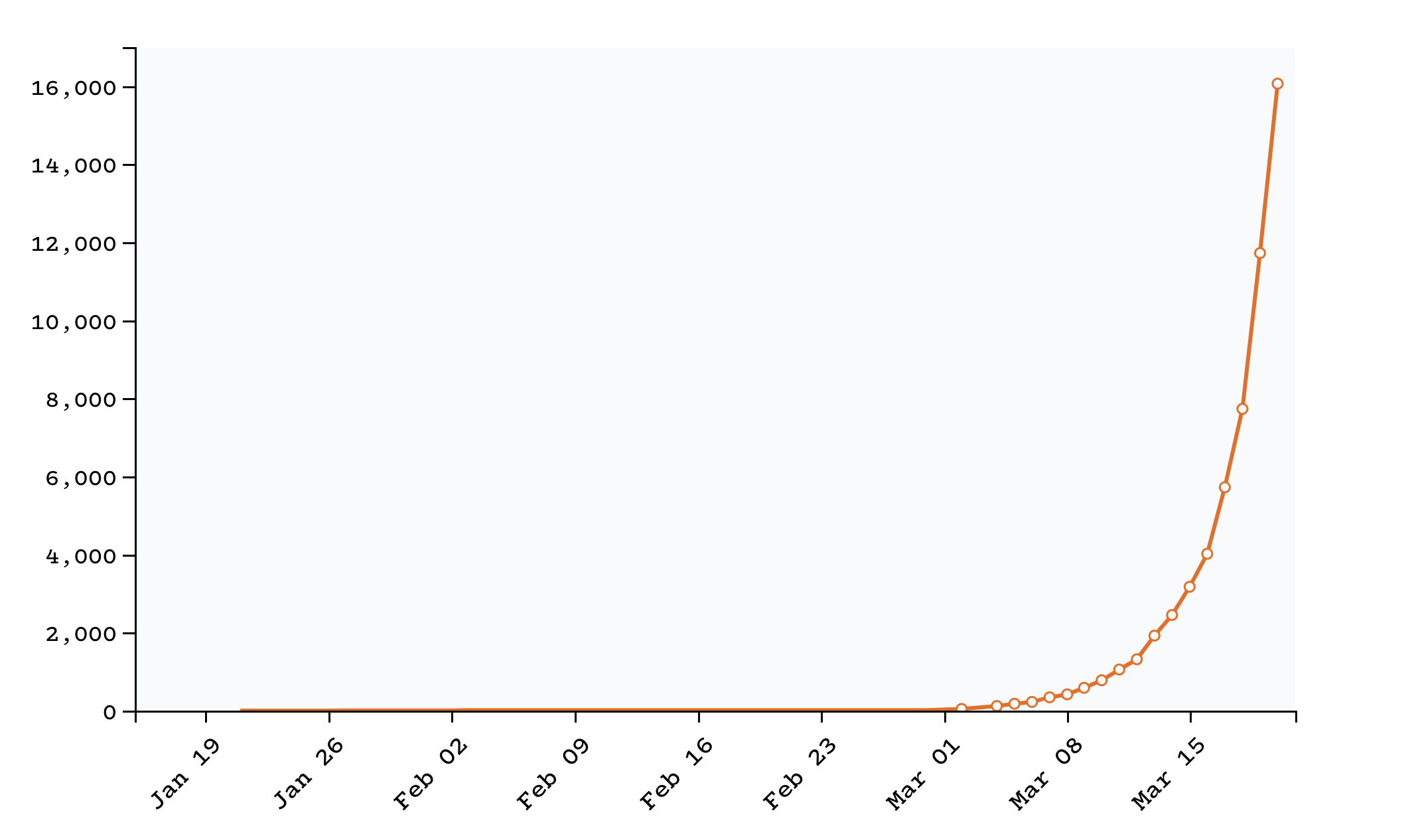
Data: The COVID Tracking Project, an ongoing investigation co-founded by The Atlantic in collaboration with more than 100 volunteers
That may sound like a lot. But experts believe that the United States still isn’t testing enough people to detect the outbreak’s true spread. The virologist Trevor Bedford has found evidence that the coronavirus began spreading in the United States in January. It has already infected approximately 87,000 Americans, he says.
Here’s what his estimate of the pandemic’s arrival in America looks like—compared with how many people we thought were sick at the time:
.png)
Data: Trevor Bedford, the Internet Archive, the COVID Tracking Project
The truth is: We don’t know how many Americans are infected with the coronavirus.
The United States is a country soon to be overrun with sick people. As the positive tests for the new coronavirus have ticked upward, so, inevitably, will the deaths.
A study published this week by Imperial College London predicted that unless aggressive action is taken, the coronavirus could kill 2.2 million Americans in the coming months. A day after that study was published, its lead researcher developed a dry cough and fever. He had COVID-19.
When Wuhan began burning with infections in December, the U.S. government took only illogical, inadequate actions to stop the virus’s spread: It banned foreigners from entering from China, but inconsistently monitored Americans returning from the country. The president laughed off the virus and the Democrats’ response to it, calling it their “new hoax,” which immediately polarized the citizenry’s response to precautionary public-health information. When the sparks of this conflagration hit, Seattle was aflame before anyone at the CDC had started to reach for water.
COVID-19 is an American catastrophe, a slow-motion disaster only now coming into view. When its true proportions have been measured, it will make the early government response look even more outrageous than it already seems. What’s happening here, in this country, was avoidable. Nearly every flaw in America’s response to the virus has one source: America did not test enough people for COVID-19.
Testing should have told doctors how to triage patients and hospitals when to prepare their wards. It should have allowed governors to gauge the severity of a local outbreak and informed federal officials as they allocated scarce masks and ventilators. Testing should have answered the all-important question in any pandemic: How many people are sick right now? Had the nation known that, the systems that were put into place over years of pandemic planning could have powered on, protecting millions of Americans and containing the illness.
Instead, the CDC botched its own test development. It sent testing kits to state public-health labs with a nonfunctioning ingredient. And by then, the virus was already spreading. It was already spreading as the Food and Drug Administration held up independent labs that had made their own tests. It was spreading as samples piled up, as the world’s top virology researchers pleaded to be permitted to test them and as the FDA denied their requests.
The virus was spreading as a delay in test kits became a national shortage. When community transmission in the United States was discovered, and states and hospitals lacked the supplies to diagnose even a dangerously ill patient, it was spreading. When a week passed, and the market began to collapse, and the country had barely tested 1,000 people, it was still spreading. Even as kits started to trickle out, the CDC and many state officials clung to restrictive rules that allowed only patients who had traveled internationally or been exposed to a known case to be tested, even though the coronavirus was already clearly spreading in American offices, day cares, and movie theaters. Doctors and nurses with all the symptoms of COVID-19 were denied tests because they could not prove exposure. The virus was still spreading.
Every six days that the country did not test, every six days that it did not act, the number of infected Americans doubled.
“The way no one expected how this response would fail in the U.S. is the testing,” Nahid Bhadelia, the medical director of the Special Pathogen Unit at Boston University School of Medicine, told us. She is an expert in infectious diseases and pandemics, and oversees the medical-response program at one of the few labs in the country permitted to handle the pathogens that cause Ebola, anthrax, and the bubonic plague.
“If you don’t know where the disease is early in the epidemic, you have no hope of containing it,” Bhadelia said. “Even now, [testing is] that Achilles’ heel; it’s the crack that is making its way throughout our entire response.”
Without testing, there was only one way to know the severity of the outbreak: counting the dead. On February 29, Washington State confirmed that a man who had been at the Life Care Center outside Seattle had died, the first American death officially attributed to the virus. According to a now-archived version of the CDC’s website, the United States had, by then, tested 472 total people.
The death came at the end of a month that was America’s last chance at containing COVID-19. But it was too late. February had been lost.
On the last day of January, Trevor Bedford, a scientist at the Fred Hutchinson Cancer Research Center, in Seattle, hit Publish on a 484-word blog post that should have shaken the nation.
Bedford is one of the country’s experts on the evolution and infectiousness of viruses. Virus genomes are like tree rings: They provide clues to where a virus came from and how many times it’s been passed from person to person. With the outbreak raging in Wuhan, Bedford had been studying the genetic sequences of the new coronavirus that Chinese researchers had posted. By January 11, six were in the record, which allowed him to reconstruct the relationships between the individual strains. Though the World Health Organization insisted that this new coronavirus had “limited human-to-human transmission,” the genomes told Bedford otherwise. Whatever this virus was, he suspected it could spread easily among strangers, like the common cold or the flu.
Six days later, when a pair of travelers in Thailand came down with a similar illness, and researchers published the genome of the virus that had infected them, Bedford’s worst fears were confirmed. An epidemic had already begun. The new coronavirus had slipped the cordon in Wuhan, and was out in the world.
“As this became clear to me, I spent the week of Jan 20 alerting every public health official I know,” Bedford wrote that month. On January 23, the Chinese government, which had spent weeks trying to cover up the virus, swung into action. It locked down the city of Wuhan and by mid-February had restricted the movement of 700 million people. On January 24, the CDC announced it had developed a test for the disease. The FDA wouldn’t approve it for another week and a half.
This was the moment that epidemiologists had spent years dreading and anticipating. Almost every city and state in America had a pandemic-preparedness plan, reams of paper ready to put into action.
King County, in which Seattle and Kirkland sit, had a plan, of course. The last revision, dated October 2013, forecast the consequences of a pandemic flu in now-eerie detail. The country, they predicted, would be faced with deaths that could range into the millions. The pandemic “has the potential to suddenly cause illness in a very large number of people, who could easily overwhelm the healthcare system throughout the nation.” No vaccines would be available at first. Community services could break down. Everything could become disrupted “for several weeks, if not months.” So many of the steps that then seemed unthinkable to regular people—closing schools for months, social distancing, curfews, and more—were not only contemplated but gamed out.
Except for one thing. The plan took as a given that a functional testing apparatus would catch diseases on the way in, or at least before the fire started raging. Under its “Planning Assumptions” section, the second bullet point read, “There will be a need for heightened global, national and local surveillance.” Surveillanceis public-health jargon for testing and the system that surrounds it. The planners knew there would be a need; they barely considered that it would not be met.
“A heightened local surveillance system … serves as an early warning system for potential pandemics and a critical component of pandemic response plans,” they wrote in another section of the report. “Local surveillance during a pandemic outbreak provides important information regarding the severity of disease, characteristics of the affected population, and impacts on the healthcare system.”
For every contingency that was considered, every difficulty and problem was assumed to be downstream of the high-quality information that would flow from the testing system. Without data about American cases in hand, how to handle the virus would become a matter of guesswork, not judgment.
In late January, as Bedford began to warn public-health officials, there remained, according to the president, nothing to worry about. “We have it totally under control,” President Donald Trump said at Davos. “It’s one person coming in from China, and we have it under control. It’s going to be just fine.”
On or about January 15, someone infected by the coronavirus arrived in the Seattle area, Bedford’s research would later show. The virus began to silently spread in the region. It would not be detected for another six weeks.
If there is one thing about the novel coronavirus that you must understand, it’s that it is a firecracker with a long fuse. Here is what the explosion looks like: Every six days, the number of people infected by the disease doubles, according to estimates from Bedford and other epidemiologists. At the start of February, Bedford now believes, the United States had something like 430 infections; if American interventions have done nothing to slow the disease’s spread, then his simple calculations show that more than 120,000 people could be infected by this weekend. Because of the great uncertainty, it’s probably most appropriate to give Bedford’s range: About 60,000 to 245,000 people are now infected with COVID-19 in the United States.
An invisible fuse sets off this burst of disease. If someone is infected with the coronavirus on Monday, she may start being contagious and infecting other people by Wednesday. But she may not start showing symptoms until Friday—meaning that she was spreading the virus before she even knew she had it. And in some cases, infected people take 14 days to start showing symptoms.
The onset of symptoms starts another awful clock. Many people will recover in a few weeks. But if someone’s case is severe, he may not recover for a month. And even if someone’s case is fatal, she may still survive for three weeks. This means that, first, cases discovered now may not become deaths for weeks; second, some people who will die in early April may only start showing symptoms today.
Mitigation efforts must burn through the same fuse. Even the decision to lock down the Bay Area, the country’s richest region, will not relieve pressure on the medical system for weeks.
Both of these factors mean that time is of the essence. This virus hides effectively and doubles quickly, but it kills slowly and painfully, and it kills most effectively when medical care isn’t available. This makes the coronavirus a particular disaster for the American hospital system, which after decades of streamlining has little spare capacity.
If the coronavirus was in the United States, it had to be found early, before too many explosions could go off.
Helen Y. Chu, an infectious-disease specialist at the University of Washington, thought she had a way to detect COVID-19’s arrival. She directed a monitoring program called the Seattle Flu Study, which studied the spread of the seasonal flu and collected samples from sick people on an ongoing basis. What if some of those patients didn’t have the flu at all, but COVID-19? In January, she and her colleagues began asking federal and state officials for permission to repurpose specimens to test for this other, similar respiratory disease, according to The New York Times. They turned her down then—and they kept rejecting her requests as the weeks wore on. There were legitimate privacy concerns, and government officials were not ready to authorize Chu to look.
On the last day of January, roughly 380 people were already infected with the coronavirus, most of them in the Seattle area, according to Bedford’s estimate. (Bedford is also part of the Seattle Flu Study.)
But then the CDC hit a disastrous roadblock, as it began to send test kits to public-health labs across the country. Two of the test’s reagents were fine, in most cases, but a third chemical initially deemed necessary for the test simply did not work. For the time being, every test for COVID-19 would have to be conducted by the CDC.
As the CDC struggled to find a solution, other laboratories tried to bring their own tests online. They found themselves hamstrung by the FDA, which, though it repeatedly loosened the rules, could not move as fast as the coronavirus.
Alex Greninger, the assistant director of the clinical virology laboratory at the University of Washington, wanted to run a test of the lab’s own design. His lab would end up being one of the fastest to set up testing, and become the most important early source of information about the growth of the outbreak. But initially he, too, found himself caught up in the bureaucratic gears. On February 14, he sent a frustrated email to other clinical laboratories. The obstacles to setting up a test were unbelievable, he wrote: The FDA was asking him to show test results for more specimens than there were confirmed coronavirus cases in the United States—and the FDA wasn’t even making samples from those cases available to him. (The FDA did not immediately respond to The Atlantic’s request for comment.)
No one at the federal level was moving fast enough to actually deal with the looming disaster. “The most pernicious effect of the current regulatory environment is that it kneecaps our ability for preparedness should a true emergency emerge,” Greninger wrote to other laboratory directors. “Why bother getting ready as a clinical lab if you think that you won’t ever be allowed to do anything until May or June?” Even after his lab got FDA approval, another two to three weeks would pass before it could actually test a large number of samples. In coronavirus time, three weeks is about how long it takes for 100 cases to become more than 1,000. “We’ve been exceptionally fortunate to have so few positive cases,” he wrote. “Should that change in the coming weeks, this month will have been the time when we could have expanded our capacity for testing by including clinical labs.”
But the entire American testing effort, which would provide the crucial surveillance capability to understand any incipient outbreak, had stalled. The days ticked by; the virus spread. American public-health labs—which generally have far more capacity than the CDC—had completed only 16 tests, maybe a handful of people, by mid-February. All the way to February 26, only 102 specimens, or perhaps 50 people, had been tested by those labs. Overall, the CDC had tested fewer than 500 people. If the U.S. had a small number of cases, it was only because no one was looking for them. “We just twiddled our thumbs as the coronavirus waltzed in,” William Hanage, a Harvard epidemiologist, wrote in The Washington Post.
Perhaps because of the wildly constrained supply of tests, the criteria to get one were strict. You basically had to go to Wuhan, lick someone, and then develop pneumonia. No one from the federal government even tried to look for community transmission in the United States. In late February, the president voiced his hopes that “the numbers are going to get progressively better as we go along.”
They would not. In fact, as Trump spoke, the virus had reached a nursing home in the Seattle suburb of Kirkland, where it has so far killed 35 residents. The staff knew a mysterious virus was circulating, but life went on as normal. A concerned visitor who had gone to a Mardi Gras party at the center reached out to King County Public Health, the Los Angeles Times reported, and got the runaround.
On February 26, the CDC confirmed what should have been clear much earlier: Community transmission in the United States had begun. The coronavirus was now spreading among Americans who had not traveled abroad or known a confirmed case. At least 60 people in the country now had the virus, according to the CDC’s totals at the time—and, as researchers and analysts soon realized, the true number was almost certainly much higher.
The CDC’s website now says that there were already 268 cases in the United States by that date. When Japan had nearly as many confirmed cases, it closed every school in the country. But because of the testing backlog, the United States remained unaware of its infection rate. And the president encouraged happy thinking. As CDC officials warned that the number of cases could soon quickly rise, Trump disagreed. “Within a couple of days,” he said, the number of cases “is going to be down to close to zero. That’s a pretty good job we’ve done.”
Bedford now estimates that roughly 7,640 people in the United States were already infected.
Chu, the Seattle infectious-disease specialist, decided not to wait for government officials any longer. As the United States declared the first cases of community transmission, she tested through Greninger’s lab without official approval and got a positive. The meaning was obvious to her. “It’s just everywhere already,” she later told The New York Times.
Under pressure to get tests out, the most important fix that our national agencies could make was to simply allow labs to start testing people. In a description that has now been removed from the CDC’s website, the agency gave labs simple instructions: They should use the two working reagents in the old kits. These instructions could have gone out weeks before they actually did, Greninger says, because they relied on the supplies that the CDC had already sent.
Meanwhile, Bedford began examining the new coronavirus strains from patients in Washington State, just as he had, six weeks earlier, analyzed the Asian samples. The Seattle-area specimens led him to a devastating conclusion: The viral genomes were too similar to have arrived in the United States at different times, from different people, but they were also too varied to have arrived recently. By the end of February, the disease had not only established itself in the United States. It had been circulating for close to six weeks. Seattle, on March 1, found itself in the same position as Wuhan did on January 1, with a growing coronavirus outbreak that was on the verge of exploding.
If Seattle went the route of Wuhan, the nation had three weeks before being set on a track in which hundreds or even thousands of people might die in Washington State alone. If a fire was raging in Seattle, it would throw off sparks across the country, hitting many more.
The clock required urgent action. On March 2, Bedford pressed Seattle officials to implement social-distancing policies immediately. If the epidemic grew any further … well, the CDC knew what might happen.
“Widespread transmission of COVID-19 in the United States would translate into large numbers of people needing medical care at the same time,” the agency warned in a passage titled “What May Happen” on the coronavirus page of its website. “Public health and healthcare systems may become overloaded, with elevated rates of hospitalizations and deaths.”
One day after Bedford published his warning, the CDC announced that it would stop reporting how many people in the United States had been tested for the coronavirus. Donald Trump shared his views on Fox News the following night. “A lot of people will have this, and it’s very mild,” he said. “They’ll get better very rapidly. They don’t even see a doctor. They don’t even call a doctor.”
The virus was now clearly spreading, but the CDC still seemed stuck in neutral. On March 10, CDC Director Robert Redfield described his agency’s strategy to The New York Times. “It’s going to take rigorous, aggressive public health—what I like to say, block and tackle, block and tackle, block and tackle, block and tackle,” he said. “That means if you find a new case, you isolate it.”
Redfield’s advice would have sounded reasonable back on Planet A, where the U.S. surveillance apparatus had not failed so spectacularly, but it was almost nonsensical on Planet B, where we all now live. Almost no one was getting tested, so how could anyone find a new case? A few days earlier, a state-by-state investigation by The Atlantic found little evidence that more than 2,000 people had been tested nationwide. We also found that many states had effectively no ability to test for COVID-19, and the few that did—Washington and California—were already deep into their local outbreaks. After we published the story, reports flooded in from across the country from people who had been denied tests, or doctors who couldn’t get one for patients who they believed needed them. In some cases, even doctors who had treated COVID-19 patients were not able to get tested.
As we heard from dozens of frightened and frustrated people across the country, President Trump told reporters, “Anyone who wants a test can get a test.” This was and is still not true.
The scarcity of tests forced officials to ration them. States, counties, and hospitals implemented strict rules about who could qualify for a test. The rules, while based on CDC guidance, were often too limited, given how widely the virus had already spread: They asked about foreign travel and confirmed exposure to a COVID-19–positive patient, weeks after it was clear that the virus was in the United States and that many cases were going undetected. At least 19 stateshave used a version of the rules that made it effectively impossible to detect the first signs of community spread in a state or city.
In the few places where officials have tested people without known exposure to COVID-19, they have found the virus. In Sonoma County, California, the public-health department asked four hospitals to test the first 20 patients who walked in the door each day with any coronavirus symptoms—even if the patient had not traveled abroad or been exposed to another known case. They started the project on a Friday. They had found a positive by Saturday. “All we needed was one case to say: Yes, we have community transmission,” Jennifer Larocque, a spokesperson for the county, told us.
In other places, the criteria have prevented residents from understanding the true extent of community spread. Nebraska, which hewed closely to the rules, insisted it had only one case of community spread, even as suspicious cases filled ICUs, according to a 35-year-old doctor who asked not to be named, because she was not authorized to speak with the press. Nebraska announced its second case of community spread on Wednesday. The state has tested 800 people, total, for the coronavirus, the chief medical officer said.
The federal government’s reliance on CDC data about the severity of the outbreak froze efforts to stop it. Even after Bedford’s warning, the government published no studies of viral mutation. The void forced leaders to act on the basis of risk, not solid information. How could a mayor shut down her city if it had only 10 for-sure cases? How could a CEO tell employees to call off their trips—and not to Western Europe or central China, but to Seattle?
American cities, blinded by the lack of testing data, did little as crucial days went by. On March 7, as the severity of the local outbreak was becoming known, huge events were allowed to go on. More than 30,000 people attended a Seattle Sounders game that night. No one wanted to say what has now become clear: February was our chance to get this right. We lost that entire month. And we now live in a new era of work stoppages, overwhelmed hospitals, dead elders, and a wrecked economy.
No one had the guts to say what needed to be said over the past month: To save our people, we will have to keep our cities in a chokehold and decimate our economy. It would have taken guts and the full-throated backing of every level of government and agency, as well as irrefutable data, for local officials to do something like that. No one told them to, and the data did not exist for them to come to that conclusion on their own.
Without strong federal leadership, each state has been going after its own solutions and running its own show, as if its residents would stay neatly within their own state lines. Despite the rising number of cases and hospitalizations, President Trump tried to use partisan rhetorical tactics to fight the virus, and in so doing, encouraged Americans to ignore legitimate, dire warnings. Now, though Trump has begun to mobilize a response to the pandemic, his base has been slow to acknowledge that precautions are necessary. This dangerous remove from reality was possible for too long because of the absence of data showing how bad things already were.
Ironically, given that the debacle started with testing, it may end there as well. South Korea, which on March 1 was the site of the largest confirmed coronavirus outbreak outside of China, has aggressively tested a huge percentage of its population, and continues to screen massive numbers of people. Now, just three weeks later, new COVID-19 cases are declining, and only 102 people have diedas of Friday. Washington State, with one-seventh the population of South Korea, already has 83 fatalities. The U.S. caseload has ballooned to almost 20,000, more than twice South Korea’s total. Bedford and other experts believe that Korean-style massive-scale testing will be essential to restoring normal economic conditions. “This is the Apollo program of our times,” he said this week. “Let’s get to it.”
A week ago, an NBC reporter asked Trump during a White House briefing whether he took responsibility for the deadly testing delays. His reply was immediate: “No. I don’t take responsibility at all.”
Frankie Dintino, Quinn Ryan, Jacob Stern, and Ed Yong contributed to this report.



