DOD's plan for 'virtual critical care wards' for COVID-19 patients
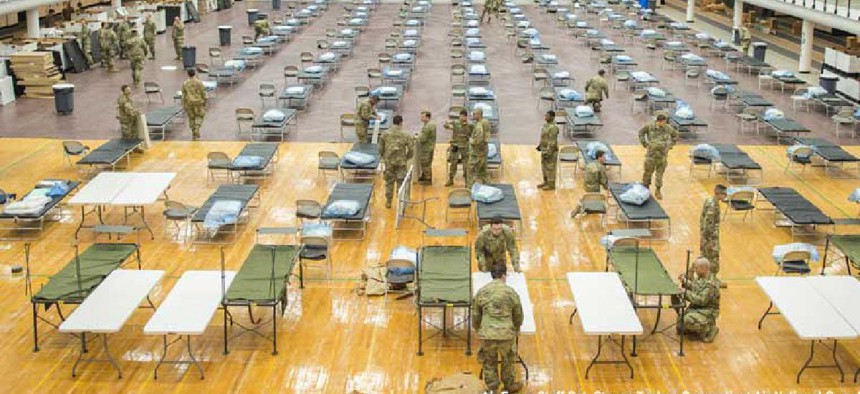
The Medical Technology Enterprise Consortium wants health professionals to be able to deliver high-quality critical care to bedsides of COVID-19 patients in field hospitals, small rural health care facilities and even gymnasiums.
What if health care professionals, instead of sending coronavirus victims to overcrowded, understaffed hospitals, could download an app, register their patients and have them admitted to a virtual ward in a temporary hospital where a teleconnected critical care team could monitor their progress via local sensors, wearables or mobile devices?
That’s the vision of the Medical Technology Enterprise Consortium, which plans build “virtual critical care wards” so health professionals can deliver high-quality critical care to bedsides of COVID-19 patients in field hospitals, small rural health care facilities and even gymnasiums. MTEC’s proposed a National Emergency Telecritical Care Network (NETCCN) would extend the geographic reach of limited critical care resources and expertise, reduce transmission caused by transferring patients between facilities and conserve personal protective equipment.
MTEC is an international enterprise research partnership between the U.S. Army Medical Research and Development Command, industry and academia dedicated to accelerating development of medical solutions for the military. It focuses on research into infectious diseases, combat casualties, clinical and medical rehab as well as on leveraging information science to improve military medical training and advance technologies that support in-theater medicine.
In a request for project proposals, MTEC describes NETCCN as “a cloud-based, low-resource, stand-alone health information management system for the creation and coordination of flexible and extendable ‘virtual critical care wards.’” It suggests that one experienced – and it stressed experienced – “virtual intensivist” could monitor and respond to emergencies for 75-125 patients while just one remote ICU nurse could provide virtual monitoring for 30-60 patients.
While telemedicine capabilities are widely available today, they tend to be difficult to scale and interoperate with other telehealth systems, partner provider-networks and tele-clinical services. NETCCN aims to leverage the same basic technologies telemedicine uses -- cellular communication networks, electronic health records systems and cloud-based information storage -- to extend high-quality, intensive critical care to non-traditional and temporary health care facilities to help manage the respiratory failure and organ dysfunction associated with COVID-19.
These virtual wards would be self-contained health information management systems that tapped into elastic cloud computing, internet of things connections and artificial intelligence to integrate audio-visual communications capabilities to manage the flow of patients and their health information.
The technology infrastructure envisioned to support the required information sharing and reporting capabilities would feature a “network of networks” governance structure to coordinate patient- and system-level data and support the ability to push training and materials to frontline clinicians who will be working beyond their normal scope of practice.
METC has $7 million in FY20 funds for the program and expects to make up to six award to qualified teams that can rapidly prototype, test and refine tele-critical care and data visualization solutions. It plans to first build a localized tele-critical care capability, which will be rolled out regionally and nationally where needed.
White papers are due April 27.


